PTSD affects how the brain responds to stress, memory, and emotional signals. These shifts can make daily life feel unpredictable and exhausting. Neurofeedback for PTSD offers a structured method of teaching the brain steadier patterns through real-time feedback. Many individuals turn to this approach when they want a clearer understanding of the neurological contributors to PTSD symptoms or when they are looking for additional support alongside traditional care.
This resource explains how trauma affects the brain, how neurofeedback therapy works, and why some people choose neurofeedback training as part of a wider recovery plan.
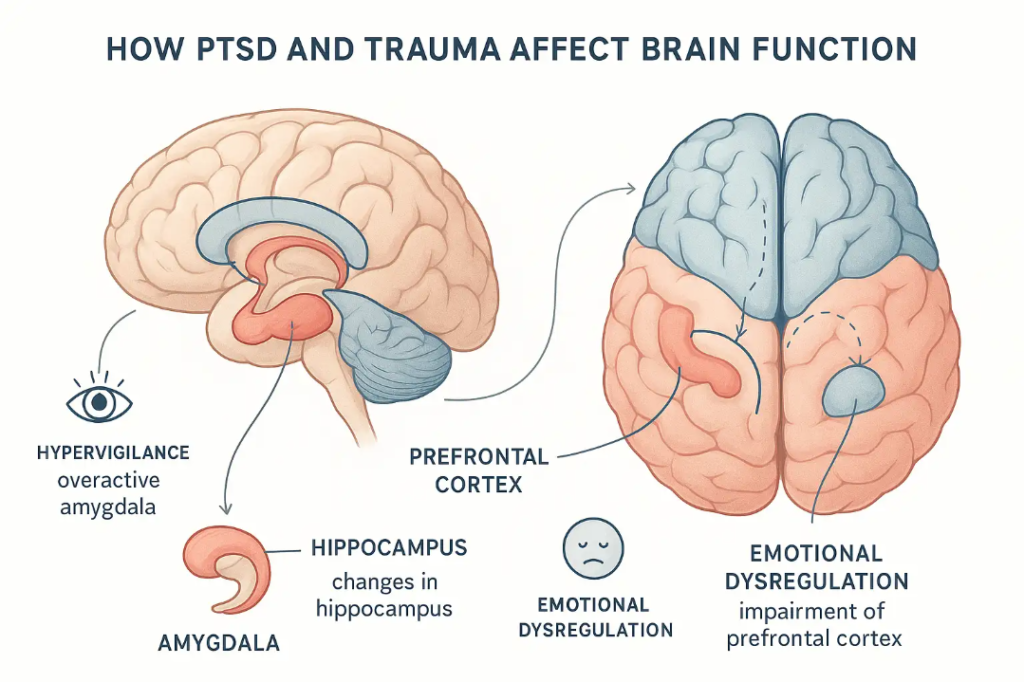
Trauma can change communication between brain regions that evaluate threat and regulate emotional responses. When someone develops PTSD, the brain may continue to react as though danger is still present. This ongoing pattern can lead to:
Research shows that areas like the amygdala may become more active, while regions responsible for calming the stress response may become less responsive. These changes often make it difficult to return to a relaxed state after a trigger.
Neurofeedback therapy aims to address these patterns by giving the brain clear information about its own activity. Through repeated training, the brain can practice returning to more balanced rhythms. Understanding these underlying disruptions helps individuals see why PTSD symptoms can persist and how targeted training may support change.
Neurofeedback therapy uses sensors on the scalp to track electrical activity in the brain. That activity is translated into visual or audio cues that guide the training process. When the brain moves toward a steadier pattern, the system reinforces that change.
For those with PTSD, this matters because emotional regulation challenges often stem from inconsistent communication between networks responsible for evaluating threat and managing responses. Neurofeedback for PTSD focuses on strengthening these regulatory pathways.
Individuals often describe gradual improvements such as:
Neurofeedback therapy is typically paired with other forms of care. It supports treatment by working at the neurological level while therapy addresses emotional processing and daily coping skills. This creates a coordinated plan that respects both the brain and the lived experience of trauma.
Complex PTSD develops from long-term or repeated trauma and can include symptoms like dissociation, chronic fear responses, and ongoing emotional distress. Because complex trauma affects several layers of brain function, individuals may feel stuck in patterns that feel difficult to shift.
Neurofeedback training offers a noninvasive way to work with these deeper disruptions. By giving the brain information about its real-time activity, training sessions help strengthen the pathways associated with calm and regulation. Over time, this repetition can support improvements in:
Many individuals value that neurofeedback does not require revisiting traumatic memories directly. Instead, it focuses on how the brain responds in the present moment. This allows patients with complex PTSD to develop stronger internal regulation skills that support progress in therapy and other forms of care.
Studies continue to examine how neurofeedback may influence PTSD symptoms, including research involving electroencephalographic neurofeedback (NFB) and functional MRI neurofeedback. Although individual responses vary, findings show promising patterns.
Research highlights include:
Trials have included both adults and children with trauma histories. Because the field is still growing, researchers continue to explore which protocols may be most effective for different forms of trauma, including complex presentations.
These findings help explain why neurofeedback treatment is often considered as part of a broader approach to PTSD recovery. While it is not a stand-alone solution, it provides an additional avenue for addressing the neurological contributors to symptoms.
PTSD treatment is most effective when it reflects the unique needs of each individual. Neurofeedback can support this personalized approach by addressing the neurological aspects of PTSD while therapy works on thought patterns, relationships, and coping skills.
Neurofeedback may be paired with:
This combination helps build a foundation for long-term progress. Neurofeedback training provides steady practice in maintaining regulated brain activity, while other approaches help individuals process experiences and develop new behavioral tools.
A coordinated plan also allows clinicians to adjust care as symptoms change. This type of flexible structure is especially helpful for complex trauma or fluctuating symptom patterns.
Neurofeedback for PTSD offers a method of teaching the brain to access calmer and more organized patterns. By focusing on real-time feedback and steady repetition, it supports emotional regulation, attention, and daily functioning. Although not a replacement for traditional PTSD treatment, neurofeedback can be a helpful addition to a thoughtful, individualized plan. If you would like to learn how neurofeedback fits within your care, Carolina Hyperbaric and Wellness can provide guidance, assessments, and information about available training options. Reach out to their team to discuss your goals and take the next step toward steadier well-being.